Persistent anal pain can affect your daily life. It may limit work, exercise, and even social interactions. If you suffer from repeated discomfort, you might have a fissure.
Chronic fissures are painful tears in the anal lining. They often resist healing and keep recurring. In this blog, we will explore why fissures return and how you can prevent them. By the end, you will understand how to manage fissures effectively and regain control of your life. Know more from Dr. Ashutosh Nayak, the best fissure doctor in Kolkata.
What Are Chronic Fissures?
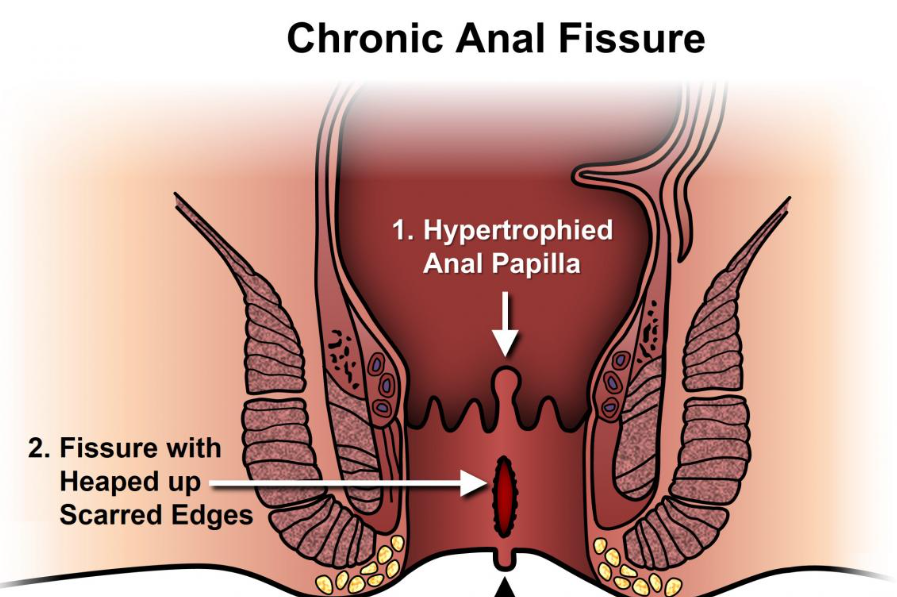
Anal fissures are small tears in the tissue lining the anal canal. Acute fissures heal within a few weeks. Chronic fissures last longer than 6–8 weeks. Scar tissue often develops, making the fissure harder to heal. Symptoms include sharp pain during bowel movements, bleeding, and itching. Recurring fissures cause anxiety and affect your quality of life.
Common Causes of Chronic Fissures
- Constipation and Hard Stools
Constipation is the most common cause of recurring fissures. Hard stools stretch the anal canal and tear the tissue. Straining during bowel movements worsens the fissure.
- Tight Anal Sphincter Muscles
A tight sphincter prevents proper healing. Muscle spasms reduce blood flow in the affected area. Less blood flow slows tissue repair and increases pain.
- Poor Hydration and Diet
Low water intake and fibre-poor diets create hard stools. This combination increases the risk of fissures.
- Repeated Trauma
Frequent irritation from wiping or infections can trigger fissures. Even minor trauma can prevent healing.
Symptoms You Should Not Ignore
- Sharp pain during or after bowel movements
- Bright red blood on toilet paper or stool
- Itching or irritation around the anus
- Small lumps or skin tags near the fissure
- Persistent discomfort or burning sensation
If these symptoms continue for weeks, consult a specialist immediately. Dr. Ashutosh Nayak specialises in fissure treatment, offering tailored treatments for chronic cases.
Why Fissures Keep Coming Back
- Scar Tissue Formation
Scar tissue develops at the fissure site, reducing tissue elasticity. Less elasticity means the tissue tears again during bowel movements.
- Recurrent Constipation
Without addressing bowel habits, fissures tend to recur. High-fibre diets and hydration prevent hard stools and constipation.
- Muscle Spasms
Chronic sphincter spasms prevent blood flow. This slows healing and increases recurrence risk.
- Ignoring Early Symptoms
Ignoring minor tears or using only home remedies allows fissures to worsen.
Risk Factors That Increase Chronic Fissures
- Age and Tissue Elasticity
Older adults have less flexible tissue, which delays healing. Fragile tissue tears more easily.
- Sedentary Lifestyle
Lack of exercise reduces bowel movement regularity. This leads to constipation and fissure recurrence.
- Certain Medical Conditions
Conditions like Crohn’s disease, ulcerative colitis, or diabetes increase chronic fissure risks.
- Poor Bathroom Habits
Straining or prolonged sitting on the toilet damages anal tissue. Regular bowel habits prevent this risk.
- Medications
Some medications, like painkillers or anti-depressants, cause constipation. This indirectly contributes to chronic fissures.
Effective Medical Treatments for Chronic Fissures
- Topical Ointments and Medications
Doctors prescribe nitroglycerin ointments or calcium channel blockers. These relax the anal sphincter. Improved blood flow accelerates healing. Pain relief creams reduce discomfort during bowel movements.
- Non-Surgical Interventions
Botox injections temporarily relax the sphincter muscles. This technique helps fissures resistant to conventional treatment. It is minimally invasive and highly effective.
- Surgical Options
Lateral internal sphincterotomy involves making a small incision in the anal sphincter. This reduces muscle tension and allows the fissure to heal. Surgery is recommended for fissures that do not respond to conservative care.
- Fissure Plug or Advancement Flap
In severe cases, doctors may recommend a tissue flap to cover the fissure. This protects the area and promotes healing.
Lifestyle and Home Strategies
- High-Fibre Diet

Fibre softens stool, reducing strain during bowel movements. Include fruits, vegetables, oats, and whole grains.
- Adequate Hydration
Drink at least 8–10 glasses of water daily. Hydration prevents hard stools and constipation.
- Regular Exercise
Exercise improves bowel function and reduces sphincter tension. Even daily walking helps.
- Gentle Anal Care
Use soft toilet paper or wet wipes. Avoid harsh soaps and vigorous scrubbing.
- Warm Sitz Baths
Soaking in warm water for 10–15 minutes relaxes anal muscles. This improves blood flow and reduces pain.
- Stress Management
Stress worsens sphincter spasms and delays healing. Practice yoga, meditation, or deep breathing exercises.
- Tracking Bowel Movements
Keeping a log of bowel movements helps identify patterns causing fissures.
When to See a Specialist
Seek expert care if pain lasts more than two weeks. Bleeding, severe discomfort, or recurring fissures require attention. Dr. Ashutosh Nayak, the best fissure doctor in Kolkata, offers the most effective treatments. Early consultation ensures faster recovery and prevents recurrence.
The Role of a Specialist
A qualified doctor identifies underlying causes. They recommend a combination of treatment, lifestyle changes, and preventive strategies. Experts like Dr. Ashutosh Nayak tailor interventions for each patient. Chronic fissures require precise diagnosis and a structured treatment plan.
Seek Early Treatment
Chronic fissures can disrupt daily life if untreated. Understanding causes, symptoms, and treatments is critical. Combine medical care, lifestyle adjustments, and preventive strategies to achieve long-term healing.
Consult an Expert
Don’t let anal pain control your life. Schedule a consultation with Dr. Ashutosh Nayak the best fissure doctor in Kolkata for affordable treatment with Swasthya Sathi facilities.
People Also Ask
1. What causes chronic anal fissures?
Repeated constipation, tight sphincter muscles, and poor bowel habits cause them.
2. How long does a fissure take to heal?
Healing can take 6–8 weeks with proper treatment and care.
3. Can diet prevent recurring fissures?
Yes. Fibre-rich foods and proper hydration reduce recurrence risks.
4. When is surgery necessary for anal fissures?
Surgery is required if conservative treatments fail to heal chronic fissures.
5. Are there non-surgical treatments for chronic fissures?
Yes. Topical ointments and Botox injections often heal stubborn fissures.
6. Can anal fissures be prevented completely?
While prevention isn’t always possible, maintaining a healthy diet and bowel habits reduces the risk of fissures.
7. How can I relieve pain from an anal fissure?
Pain can be relieved with sitz baths, over-the-counter ointments, and stool softeners to avoid straining.
8. Is there a connection between haemorrhoids and anal fissures?
Yes, both can cause pain, bleeding, and discomfort, but they are different conditions. Haemorrhoids are swollen blood vessels, while fissures are small tears in the skin.
9. Can I exercise with an anal fissure?
Light exercise, such as walking, can help maintain regular bowel movements and reduce strain. Avoid heavy lifting or straining until healed.
10. What are the signs that an anal fissure has become infected?
Signs of infection include increased redness, warmth, swelling, pus drainage, and worsening pain. Consult a doctor if these occur.